3 Things to Do If You’ve Been Diagnosed with IBS
Written by: Marisol Teijeiro N.D. (inactive).
Medically reviewed by: Victoria Williams R.H.N.
Est. reading time: 13 minutes.
Bowel movements, defecation, going poo… it’s the #1 most important process of the human body, and not the #2! Are you one of the 14-20% of the world population with irritable bowel syndrome (that’s approximately one BILLION people!)1? It is hypothesized that those who have gotten the diagnosis are only the tip of the iceberg, meaning that there are so many more people that have it but haven’t been diagnosed yet. You know all too well how it can negatively affect your life.
Here are the first 3 things you need to do to take control of what is happening to your body. It has to do with 3 “s” words, and sh*t isn’t one of them… Stools, stress and sleep.
What is Irritable Bowel Syndrome?
Irritable bowel syndrome is a chronic, long term, recurring functional condition, meaning that when you are tested via labs or colonoscopy, everything looks normal. There seems to be no reason for your symptoms, nevertheless you have them and they are debilitating.
The Frustration of an Irritable Bowel Syndrome Diagnosis
This is extremely frustrating to hear from your doctor, especially after you have been suffering with these symptoms that have had a detrimental impact on all aspects of your life. From limiting your social life for fear of an adverse bowel movement, to affecting your work life by causing you to spend too much time in the bathroom or taking more sick days than the norm. Not to mention huge psychological impact on your well being, living with this ever growing problem.
What are the Risk Factors for Irritable Bowel Syndrome
The most noted risk factors for irritable bowel syndrome are being a women, of young age, and having a preceding gut infection of some sort2. The risk is actually four times higher for those who have had an infectious gut condition3.
Symptoms of Irritable Bowel Syndrome
The most common symptoms of IBS include a combination of recurring:
- Abdominal pain
- Distension, bloating and gas
- Abnormal bowel movements – diarrhea and/or constipation
The Categories of Irritable Bowel Syndrome
It is classified in three categories – constipation, diarrhea or an alternation between both.
- IBS-C: Predominantly constipation
- IBS-D: Predominantly diarrhea
- IBS-M: Mixed, alternating between constipation and diarrhea
- IBS-U: Unclassified
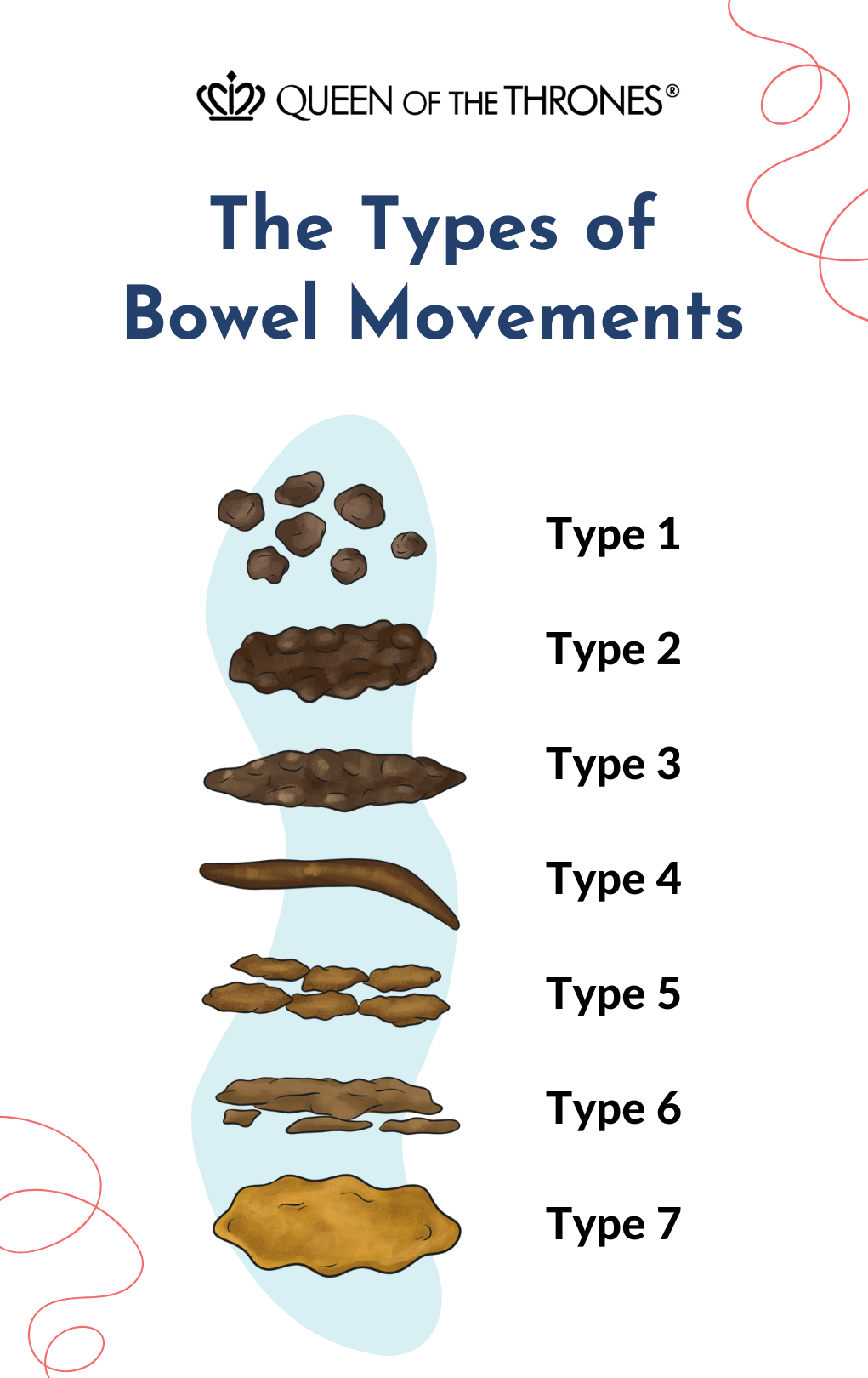
The classification is based upon the Bristol Stool Scale (see below), designating the form of bowel movements.
Is Irritable Bowel Syndrome Genetic?
It is possible. There is a link to early life exposure to stress affecting the body’s natural response to stress. So, your exposure to stress in utero or fetal programming4 as well as experiences as a young child can pre-program you into a maladaptive, unhealthy response to stress, changing the way that your hypothalamic-pituitary-adrenal axis (HPA) functions5. These are the master organs that balance the regulation systems of your body, most responsible for the way your body deals with stress.
IT IS NOT YOUR FAULT, BUT IT IS UP TO YOU TO DO SOMETHING ABOUT IT.
The Regulatory Systems Impacted In Irritable Bowel Syndrome
When you are under stress, whether it be emotional or physical stress, the body does not have the ability to differentiate6. Two processes occur in the body to try and maintain balance. The inflammatory arm of the immune system activates to try and burn off the stressor. The hypothalamic-pituitary-adrenal axis (a combination of the hormonal and nervous system7) also activates to turn off less important mechanisms that don’t deal with immediate life right now.
These three regulatory systems of the body, the immune, nervous and hormonal system’s goal in health is to keep everything in balance, everything functioning well. But under stress, they shut down non-vital functions for preservation of life. Therefore there’s dysregulation in these systems with IBS8. We also see an elevation of glucocorticoids and inflammatory markers.
So don’t be surprised if you find yourself with multiple conditions on top of your IBS. For me, I had both irritable bowel syndrome as well as polycystic ovarian syndrome (PCOS). These are often conditions that respond to an elevation of the body’s immune inflammatory messengers and the neurohormonal glucocorticoids.
Hormone Problems and IBS
Is this a coincidence then, that many women who have IBS also have PCOS? No it is not, because the body can only balance so much. In PCOS there are elevated levels of leptin, a hormone that affects food intake, energy balance and fat tissue stores but is also pro-inflammatory to the intestinal tract. Research shows that with irritable bowel syndrome there is also this elevated level of leptin in the intestine9.
When there is stress, many of our non-vital systems like being fertile, having regular periods, or having a healthy metabolism go into preservation mode, because the infinite intelligence of our bodies doesn’t want to use up resources because it has no idea how long the stressor will last.
Another co-existing hormonal problem that is common with IBS type symptoms, like constipation, is hypothyroid10.
Immune System Problems and IBS
The immune system is regulated by the microbiome. The ever important home of billions of bugs that live on our mucosal membrane and skin.
Healthy, friendly probiotics help to improve the mucosal immune system11, whereas conbiotics™, as I like to call them, or pathogenic bacteria cause total dysfunction of the immune system12.
This leads you susceptible to constantly getting sick. Overreacting to foods as your gut’s reaction to foods is based on the immune system. It is well known that people with IBS react to many foods such as lactose13, gluten14 and other components of wheat to name a few.
Nervous System Problems and IBS
Google IBS and you will soon find many links that discuss the coexistence of depression and anxiety with IBS, but also as a coexisting factor with most chronic conditions. Many say that it may be in response to the condition, but it very well may be the cause of the condition, (is it the chicken or the egg, which came first?) as stress significantly alters the bodies’ regulatory homeostatic mechanisms15.
Is Stress the Cause of IBS?
Stress is a root cause of many conditions and chronic diseases. It is likely that it is a root cause of IBS, as the overlap of anxiety, depression, hormonal disturbances and immune variations are all linked to irritable bowel syndrome.
Treatments for Irritable Bowel Syndrome
It’s no surprise that at present the majority of treatments and medicines for irritable bowel syndrome are tools that mediate the functions of these three regulatory systems of the immune, nervous and hormonal systems, as the gut is the main hub for all three.
Antidepressants and anti-anxiety medications have been used for IBS, as well as antibiotics such as Rifaximin, as a way to improve the gut microbiome16.
Fix the Foundation, Don’t Palliate the Problem
The 3 easy steps to alleviate IBS:
1. Know Your Stools:
Your stools say everything about you. It’s no surprise that irritable bowel syndrome is classified based on the form according to the Bristol Stool Scale and frequency.
They can tell you key nutrient deficiencies, like magnesium being low in hormonal problems or zinc deficiency in nervous system problems, as an example. They tell about B-vitamins and other necessities to keep the foundation of our bodies functioning in harmony.
Download the free eGuide called the 50 Shades of Poo that is the first step in understanding what your poo says about you. This will set you up with an excellent practice so you can take control of your irritable bowel syndrome!
This is the most important place to start, because as Maya Angelou said, “When you know better, you do better.” It’s time for you to know better.

2. Address Your Stress:
Stress plays such a key role in IBS and the problem is we are constantly bombarded with stress. Massages and acupuncture are great ways to balance our stress levels, but we can only do them from time to time because cost is prohibitive and we are so busy, it’s hard to go to an appointment.
A Castor Oil Pack is a legendary health practice that has been in existence since biblical times and practiced by all systems and cultures of medicine. Indian, Chinese, Greek, Mediterranean, Caribbean, etc.
This tool is predominantly used to practice the pause, or the relaxed state17. In the relaxed state you can heal. Your gut microbiota is healthier, your inflammation is down, you cleanse better and your bowels move (these are also all the things the Castor Oil Pack does, independently of helping you to practice the pause).
If you feel like you’re doing everything else ‘right’ – a healthy diet, good quality supplements, regular exercise, etc. but still feel like crap, this modernized ancient health tool can help pull everything together.
3. Fix your Sleep:
Sleep resets the body and it undeniably helps with cleansing and calming, so that the nervous, hormonal and immune systems have a fighting chance.
One way to improve your sleep is simply by wearing an eye mask. Like the Castor Oil Pack for Liver, an eye mask may help stimulate the pituitary gland to produce melatonin naturally18. This is a supplement-free way to help your body sleep.
The Queen of the Thrones® Castor Oil Eye Compress Kit contains an eye mask with a bottle of organic Castor Oil that can be applied to the eyelashes, eyebrows and delicate skin around the eyes which may help reduce the appearance of aging and wrinkles.

The Royal Flush Challenge with Recipes to Help Support IBS:
We all need a good flush from time-to-time, and the Royal Flush is a super easy way to get your system back into flow, especially if you suffer with IBS.
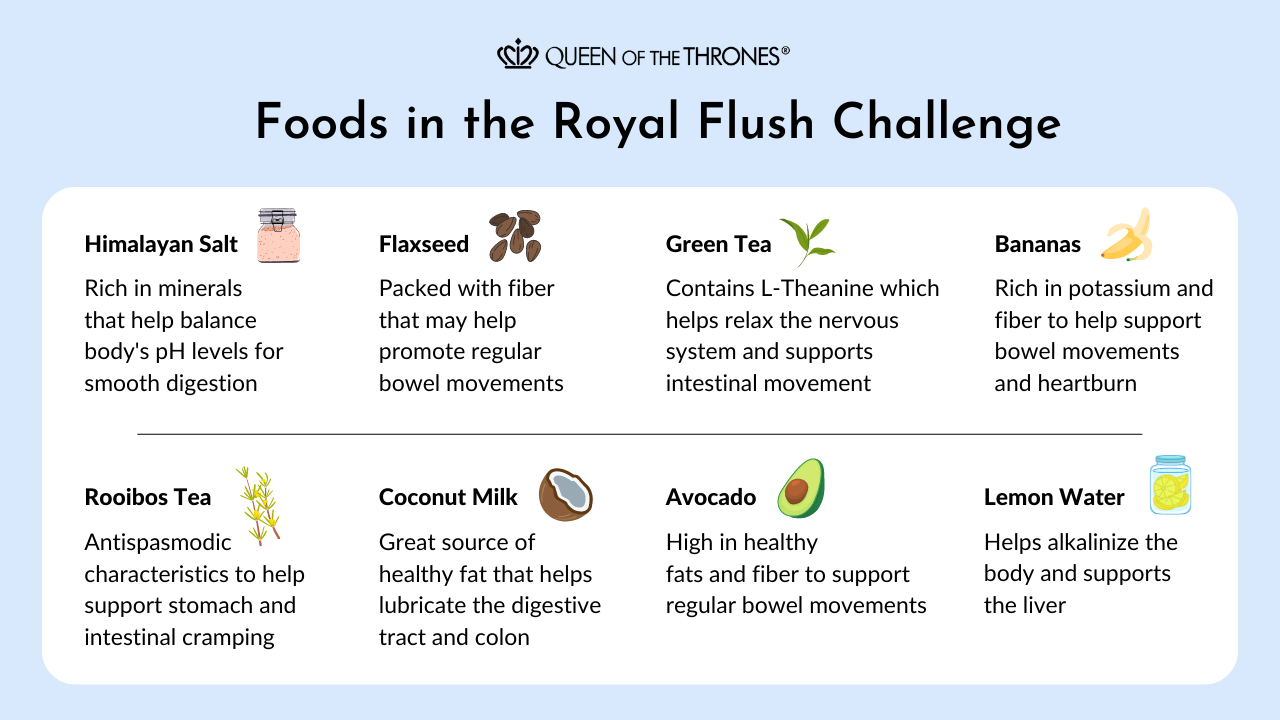
All you have to do is follow these 3 steps for 3 days! How easy is that?
Step 1: Morning Routine – Salt Water Flush
Ingredients:
- 500mL of warm water
- Juice of ½ a lemon
- ¼ tsp of Himalayan salt
Directions:
- When you wake up in the morning, pour yourself 500 mL or about 2 cups of warm water.
- Then just mix in the juice of ½ a lemon with ¼ teaspoon of Himalayan salt and drink!
Tip: Warm water and lemon is always a good way to start your day even when you’re not trying to flush!
Step 2: Mid Day Routine – Coconut Detox Smoothie
Ingredients:
- 1 tsp of freshly ground flax seeds
- ½ cup of canned coconut milk
- ¼ avocado
- 1 small banana
Directions:
By midday you’re ready for a delicious treat to fill your empty belly!
- So gather 1 teaspoon of freshly ground flax seeds, ½ cup of canned coconut milk, ¼ an avocado, and a small banana.
- Toss all of this into a blender, blend until it’s creamy smooth and enjoy!
Step 3: All Day Long Teas
Choose from:
- Green tea (this contains caffeine, so only drink it before 4pm)
- Rooibos tea (caffeine-free, so you can drink it all day)
Directions:
Drinking tea throughout the day will keep you hydrated as well as help you flush. So, drink a minimum of about 4-6 cups per day of green and rooibos teas. Another way to make sure you’re getting enough is to aim for 30mL of water per kg of body weight (or per 2.2 lbs).
So there you have it. Those are the first three things you can do once you know you have been diagnosed with irritable bowel syndrome. My hope is that you take these and let them help you to make a difference in your life. Because you don’t need to suffer. You need to learn and do what will help you to get your best body balance.
Are you a practitioner, health coach or wellness influencer? If you’re interested in recommending our easy-to-use tools and practically applying them in your health and wellness professional practice, in clinic, or online with the people you serve, you can join now!
Click here for references
1 Padhy SK1, Sahoo S1, Mahajan S1, Sinha SK2. Irritable bowel syndrome: Is it “irritable brain” or “irritable bowel”? J Neurosci Rural Pract. 2015 Oct-Dec;6(4):568-77. doi: 10.4103/0976-3147.169802.
2 Paul Enck,1 Qasim Aziz,2 Giovanni Barbara,3 Adam D. Farmer,2 Shin Fukudo,4 Emeran A. Mayer,5 Beate Niesler,6 Eamonn M. M. Quigley,7 Mirjana Rajilić-Stojanović,8 Michael Schemann,9 Juliane Schwille-Kiuntke,1 Magnus Simren,10 Stephan Zipfel,1 and Robin C. Spiller11 Irritable bowel syndrome Nat Rev Dis Primers. Author manuscript; available in PMC 2016 Aug 26.Nat Rev Dis Primers. 2016; 2: 16014.PMID: 27159638
3 Fabiane Klem,1,2,* Akhilesh Wadhwa,1,* Larry Prokop,1 Wendy Sundt,1 Gianrico Farrugia,1 Michael Camilleri,1 Siddharth Singh,3 and Madhusudan Grover1,# Prevalence, Risk Factors, and Outcomes of Irritable Bowel Syndrome After Infectious Enteritis: a Systematic Review and Meta-analysisGastroenterology. 2017 Apr; 152(5): 1042–1054.e1.PMID: 28069350
4 Mariann A. Howland,1 Curt A. Sandman,1 and Laura M. Glynn1,2 Developmental origins of the human hypothalamic-pituitary-adrenal axisExpert Rev Endocrinol Metab. 2017 Sep; 12(5): 321–339.PMID: 30058893
5 Miranda van Bodegom, Judith R. Homberg, and Marloes J. A. G. Henckens* Modulation of the Hypothalamic-Pituitary-Adrenal Axis by Early Life Stress Exposure. Front Cell Neurosci. 2017; 11: 87. 10.3389/fncel.2017.00087PMID: 28469557
6 Vanja Duric, * Sarah Clayton, Mai Lan Leong, and Li-Lian Yuan Comorbidity Factors and Brain Mechanisms Linking Chronic Stress and Systemic Illness Neural Plast. 2016; 2016: 5460732. PMID: 26977323
7 Kate Ryan Kuhlman,1 Jessica J. Chiang,2 Sarah Horn,3 and Julienne E. Bower1 Developmental psychoneuroendocrine and psychoneuroimmune pathways from childhood adversity to disease Neurosci Biobehav Rev. Author manuscript; available in PMC 2018 Sep 1.Neurosci Biobehav Rev. 2017 Sep; 80: 166–184.PMID: 28577879
8 O’Malley D1. Endocrine regulation of gut function – a role for glucagon-like peptide-1 in the pathophysiology of irritable bowel syndrome. Exp Physiol. 2019 Jan;104(1):3-10. doi: 10.1113/EP087443. Epub 2018 Dec 10.
9 De-Rong Liu, Xiao-Juan Xu, and Shu-Kun Yao Increased intestinal mucosal leptin levels in patients with diarrhea-predominant irritable bowel syndrome World J Gastroenterol. 2018 Jan 7; 24(1): 46–57.PMID: 29358881
10 Anant D. Patil Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014 May-Jun; 18(3): 307–309.PMID: 24944923
11 Salvucci E1,2. The human-microbiome superorganism and its modulation to restore health. Int J Food Sci Nutr. 2019 Mar 7:1-15. doi: 10.1080/09637486.2019.1580682. [Epub ahead of print]
12 Shi N#1, Li N#2, Duan X2, Niu H1. Interaction between the gut microbiome and mucosal immune system. Mil Med Res. 2017 Apr 27;4:14. doi: 10.1186/s40779-017-0122-9. eCollection 2017.
13Bayless TM1,2, Brown E3, Paige DM3. Lactase Non-persistence and Lactose Intolerance. Curr Gastroenterol Rep. 2017 May;19(5):23. doi: 10.1007/s11894-017-0558-9.
14 Rej A1, Sanders DS1,2. The overlap of irritable bowel syndrome and noncoeliac gluten sensitivity. Curr Opin Gastroenterol. 2019 Feb 12. doi: 10.1097/MOG.0000000000000517.
15 Vanja Duric, * Sarah Clayton, Mai Lan Leong, and Li-Lian Yuan Comorbidity Factors and Brain Mechanisms Linking Chronic Stress and Systemic Illness Neural Plast. 2016; 2016: 5460732.Published online 2016 Feb 8. doi: 10.1155/2016/5460732PMID: 26977323]
16 Emanuele Sinagra, Gaetano Cristian Morreale, Ghazaleh Mohammadian, Giorgio Fusco, Valentina Guarnotta, Giovanni Tomasello, Francesco Cappello, Francesca Rossi, Georgios Amvrosiadis, and Dario Raimondo New therapeutic perspectives in irritable bowel syndrome: Targeting low-grade inflammation, immuno-neuroendocrine axis, motility, secretion and beyond. World J Gastroenterol. 2017 Sep 28; 23(36): 6593–6627.PMID: 29085207h
17 Rolls ET et all. Representations of pleasant and painful touch in the human orbitofrontal and cingulate cortices. Cereb Cortex. 2003 Mar;13(3):308-17. ( Dopamine release, Limbic System of brain- Fatty Meal Satisfaction)
18 Rong-fang Hu, Xiao-ying Jiang, Yi-ming Zeng, Xiao-yang Chen, You-hua Zhang. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. Published online 2010 Apr 18. doi: 10.1186/cc8965
Disclaimer
Disclaimer: Any opinions, advice, statements, services, offers, information or content expressed or made available by third parties, including information providers, are those of the respective authors or distributors. Neither Queen of the Thrones® nor any third-party provider of information guarantees the accuracy, completeness, or usefulness of any content. This communication does not create a doctor-patient relationship. Information provided does not replace the advice of your health care practitioner. If you happen to purchase anything we promote, in this or any of our communications, it’s likely Queen of the Thrones® will receive some kind of affiliate compensation. Still, we only promote content and products that we truly believe in and share with our friends, family and patients. If you ever have a concern with anything we share, please let us know at care@queenofthethrones.com. We want to make sure we are always serving Our Queendom at the highest level.