Best Lab Tests to Help Support Your Irritable Bowel Syndrome
Written by: Marisol Teijeiro N.D. (inactive).
Medically reviewed by: Victoria Williams R.H.N.
Est. reading time: 11 minutes.
So you’ve been diagnosed with irritable bowel syndrome (IBS). Now what??
Why is IBS a Functional Bowel Movement Disorder?
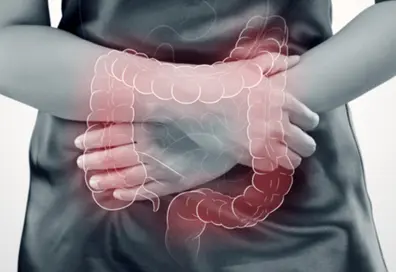
Irritable bowel syndrome is classified as a chronic functional bowel movement disorder because it is diagnosed by the symptoms that you are experiencing. These are typically abdominal pain, gas, bloating, and changes in bowel movements, often diarrhea or constipation1. Other digestive diseases that can be seen by colonoscopy or confirmed by lab tests are often excluded before IBS is diagnosed.
Why Can’t Labs Tell Me That I Have IBS?
The labs that most conventional doctors use at this moment in time don’t give a definitive diagnosis of irritable bowel syndrome. This is because it is a complex interplay of all the processes in our body. It is most often a reaction to stress in the body, whether emotional or physical, that creates an imbalance in the immune, nervous and hormonal systems.
This compounds and affects the natural digestive processes of the gut, causing inflammation, irritation, dysbiosis and lack of digestive factors that all contribute to and aggravate our symptoms2.
The big point here is that it is NOT just one thing causing IBS, and to support it you need to have a MULTIFACTORIAL approach or it just won’t work.
Why should I test for IBS?
Since irritable bowel syndrome is a chronic, long term disease, being proactive in this way helps to stay on top of things and avoid the frustration and suffering of living with uncomfortable symptoms.
It is important to do tests to rule out other conditions; when the diagnosis is clear, it is easier to direct and guide treatment and to track improvements.
Are There Functional Tests for IBS?
Yes, there are things that can be tested, but again, it is a whole-body approach.
Stress Hormone Testing Cortisol and ACTH
Research demonstrates that people with irritable bowel syndrome, mainly women, with onset at a younger age3, will have it for the greater part of their lives.
They typically also have an imbalance in their nervous system and stress response.
Stress markers of cortisol in the blood can be tested and show a difference between men and women as well as between healthy and unhealthy subjects4.
However, this is a costly test and is not common protocol for irritable bowel syndrome.
These tests are offered on YourLabWork.com.
Sleep is often something that is a complaint for women with IBS and there seems to be a difference between the type, whether it be IBS-D (diarrhea predominant) or IBS-C (constipation predominant)6. Sleep is something that normally balances our regulatory systems as it helps to reset the immune, nervous and hormonal systems.
Wearing an eye compress to bed at night may help support natural melatonin production, without having to take a supplement7. Would you love to have your own sleep compress so you can sleep better naturally?
The Queen of the Thrones® Castor Oil Eye Compress Kit uses Castor Oil applied around the eyes, eyelashes and eyebrows, covered by a sleep mask. This may help relax your system so you can get a good night’s sleep.
Inflammation Testing in IBS
Inflammation is a key component in IBS. Inflammation may be sourced from food sensitivities, allergies and intolerances, or choices of food, such as fermented foods that have high levels of histamine and act as an irritant to the gut. Inflammation is a root cause of all diseases and when there is imbalance in any system there is always inflammation.
Ferritin, the storage molecule for iron can also be a key indicator of acute inflammation. It is important to test in combination with a complete blood count (CBC) as well as an iron panel to make sure you rule out any other reasons for an elevated level of ferritin.
There are certain key markers that are indicative of inflammation. Firstly, high sensitivity C reactive protein (HS-CRP). This marker is not often tested, however, levels have been noted to be higher in those with irritable bowel syndrome as compared to the healthy population8.
Cholesterol is also one of the markers of inflammation.
A complete blood count (CBC) is always important to do as well, because it demonstrates a variety of markers. With regards to inflammation, eosinophils are a marker of allergy and when they are elevated it’s an indicator that there is elevated histamines in the body10.
It’s most commonly correlated to parasite infection, which is something to be considered in irritable bowel syndrome, since the onset of IBS can be due to a gastrointestinal infection11.
Food sensitivity testing is in a class of its own. It can demonstrate inflammatory processes in the gut as well as immune reactivity. When aiming to fix an irritable bowel, it’s important to understand that there are so many things that can be irritating it.
Food is the biggest irritator and since we eat food every day, it’s very important to address this to reduce inflammation.
There are different tests for IBS, the food sensitivity testing in this lab in the US is popular to help measure your IgG reactivity levels.
Can You Test for Dysbiosis and The Microbiome?
Another test is the Organic Acids Test (OAT), which tracks overgrowth of yeasts as well as possible clostridium infections which aids in the support of people with IBS.
There are also recent novel tests that will actually classify the types of healthy v.s. pathogenic microbes in your microbiome. This research is in its infancy.
What Should You Test?
Here is a “dream” test list, so you can rule out other sources of pain in the intestine:
- BC
- Serum Electrolytes
- Liver Enzymes, ALT, AST, ALP GGT
- Urobilinogen, direct and indirect
- Blood Lipids/Cholesterol
- Albumin
- eGFR and Creatinine
- HS-CRP
- Uric acid and urea
- Iron panel including Ferritin
- TSH, Free T3, Free T4, Antibodies for Thyroid
- Dutch Hormone Test
- Food Sensitivity Testing
- OAT Test
What to Do While You’re Waiting to Get Your Tests Done?
Start working on a solution!
Start a new self-care routine so you can begin to work on the stress component by balancing your body’s stress hormones with Castor Oil Packs. They may help with inflammation, helping the body to cleanse, get the bowels moving and support pain in the gut. The Queen of the Thrones® Castor Oil Pack for Liver Kit is made with top quality organic cotton and an easy less-mess outer layer.
In addition, you can add the simple step to your sleep ritual by wearing an eye compress to bed. As mentioned before, this may help support the body’s natural melatonin production, improving quality of sleep. Get your Queen of the Thrones® Castor Oil Eye Compress Kit today.
You see, adding these two simple steps to your self-care routine may help you support your stress, address the inflammation, cleanse, poop and sleep then you will be able to get a clearer picture of what is going on.
Peek After You Poo
Another simple step you can do is start peeking at your poo. It’s important for you to see what’s going on in your toilet bowl and the best part? You’ll have a better idea of what to tell your doctor.
Because let’s face it, lab tests start to get quite expensive. For the full panel above you could be looking at anywhere between $1500-$2500 per shot, so why not learn what your poo is saying about you? It is an easy daily at-home test, totally free!
Plus, use Queen of the Thrones® Eau de Throne® Organic Essential Oil Spray the ‘After You Poo Parfum to get into the habit of peeking after you poo and allow the blend of organic essential oils to ensure that you will never be embarrassed again for the smell you leave behind!

Start today! Don’t wait for tomorrow to do what you can do today. This is your health, your life, your body and it’s time for you to know and understand what is going on.
Are you a practitioner, health coach or wellness influencer? If you’re interested in recommending our easy-to-use tools and practically applying them in your health and wellness professional practice, in clinic, or online with the people you serve, you can join now!
Click here for references
1. Bandar Mohammed Bardisi, Abdulaziz Kamal H. Halawani, Hassan Kamal H. Halawani, Aseel Hassan Alharbi, Nesma Saleh Turkostany, Taraji Saeed Alrehaili, Aisha Ahmad Radin, and Nasser Moqbil Alkhuzea. Efficiency of diet change in irritable bowel syndrome. J Family Med Prim Care. 2018 Sep-Oct; 7(5): 946–951.PMID: 30598938
2. Emanuele Sinagra, Gaetano Cristian Morreale, Ghazaleh Mohammadian, Giorgio Fusco, Valentina Guarnotta, Giovanni Tomasello, Francesco Cappello, Francesca Rossi, Georgios Amvrosiadis, and Dario Raimondo New therapeutic perspectives in irritable bowel syndrome: Targeting low-grade inflammation, immuno-neuroendocrine axis, motility, secretion and beyond. World J Gastroenterol. 2017 Sep 28; 23(36): 6593–6627.PMID: 29085207
3. Ju Yup Lee and Kyung Sik Park. Gender Difference in Functional Gastrointestinal Disorders Korean J Gastroenterol. 2018 Oct 25;72(4):163-169. doi: 10.4166/kjg.2018.72.4.163.
4. Elizabeth J. Videlock,a Wendy Shih,b Mopelola Adeyemo,a Swapna Mahurkar-Joshi,a Angela P. Presson,c Christos Polytarchou,a Melissa Alberto,a Dimitrios Iliopoulos,a Emeran A. Mayer,a and Lin Changa,* The effect of sex and irritable bowel syndrome on HPA axis response and peripheral glucocorticoid receptor expression.Psychoneuroendocrinology. 2016 Jul; 69: 67–76.PMID: 27038676
5. Patacchioli FR1, Angelucci L, Dellerba G, Monnazzi P, Leri O. Actual stress, psychopathology and salivary cortisol levels in the irritable bowel syndrome (IBS). J Endocrinol Invest. 2001 Mar;24(3):173-7.
6. Robert L. Burr, MSEE, PhD, Research Professor,a Monica E. Jarrett, PhD, Professor,a Kevin C. Cain, PhD, Research Scientist,b Sang-Eun Jun, MS, Doctoral Candidate,a and Margaret M. Heitkemper, PhD, Professora. Catecholamine and Cortisol Levels during Sleep in Women with Irritable Bowel Syndrome.Neurogastroenterol Motil. 2009 Nov; 21(11): 1148–1e97.PMID: 19573081
7. Rong-fang Hu, Xiao-ying Jiang, Yi-ming Zeng, Xiao-yang Chen, and You-hua Zhang. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. Crit Care. 2010; 14(2): R66.PMID: 20398302
8. Keren Hod, MSc,1,2 Tamar Ringel-Kulka, MD MPH,3 Christopher F. Martin, MSPH,2 Nitsan Maharshak, MD,4 and Yehuda Ringel, MD*,2 High Sensitive C – Reactive Protein as a Marker for Inflammation in Irritable Bowel Syndrome.J Clin Gastroenterol. 2016 Mar; 50(3): 227–232.PMID: 25930973
9. Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat Rev Immunol. 2015 Feb;15(2):104-16. doi: 10.1038/nri3793.
10. Church MK1. Allergy, Histamine and Antihistamines. Handb Exp Pharmacol. 2017;241:321-331. doi: 10.1007/164_2016_85.
11. Wouters MM, Van Wanrooy S, Nguyen A, Dooley J, Aguilera-Lizarraga J, Van Brabant W, Garcia-Perez JE, Van Oudenhove L, Van Ranst M, Verhaegen J, Liston A, Boeckxstaens G Psychological comorbidity increases the risk for postinfectious IBS partly by enhanced susceptibility to develop infectious gastroenteritis. Gut. 2016 Aug;65(8):1279-88. doi: 10.1136/gutjnl-2015-309460. Epub 2015 Jun 12.
12 Zhuang Guo, Jiachao Zhang, Zhanli Wang, Kay Ying Ang, Shi Huang, Qiangchuan Hou, Xiaoquan Su, Jianmin Qiao, Yi Zheng, Lifeng Wang, Eileen Koh, Ho Danliang, Jian Xu, Yuan Kun Lee, and Heping Zhang, Intestinal Microbiota Distinguish Gout Patients from Healthy Humans Sci Rep. 2016; 6: 20602.PMID: 26852926 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4757479/
Disclaimer
Disclaimer: Any opinions, advice, statements, services, offers, information or content expressed or made available by third parties, including information providers, are those of the respective authors or distributors. Neither Queen of the Thrones® nor any third-party provider of information guarantees the accuracy, completeness, or usefulness of any content. This communication does not create a doctor-patient relationship. Information provided does not replace the advice of your health care practitioner. If you happen to purchase anything we promote, in this or any of our communications, it’s likely Queen of the Thrones® will receive some kind of affiliate compensation. Still, we only promote content and products that we truly believe in and share with our friends, family and patients. If you ever have a concern with anything we share, please let us know at care@queenofthethrones.com. We want to make sure we are always serving Our Queendom at the highest level.

Fecal Calprotectin is the test to diagnose IBS, and early diagnosis and treatment can help with cure before it goes to worse.